EMPHYSEMA :
IT IS THE CONDITION OF THE LUNG CHERACTERISED BY PERMANENT DILATATION OF THE AIR SPACES DISTAL TO THE TERMINAL BRONCHIOLES WITH DESTRUCTION OF THE WALLS OF THESE AIRWAYS..
CAUSES:
CONGENITAL PRIMARY EMPHYSEMA MAY BE CAUSED BY ANTITRYPSIN DEFICIENCY.
SECONDARY TO OTHER FACTRORS LIKE CIGARETTE SMOKING,OCCUPATIONAL LUNG DISEASE,CYSTIC FIBROSIS,CHRONIC BRONCHITIS.
TYPES:
- CENTRILOBULAR
- PANLOBULAR
PATHOLOGY :
SMOKING CAUSES THE CLUSTERING OF PULMONARY ALVEOLAR MACROPHAGES AROUND THE TERMINAL BRONCHIOLES.THESE MACROPHAGES ARE ABNORMAL IN SMOKERS AND THEY RELEASE PROTEOLYTIC ENZYMES WHICH DESTROYE THE LUNG TISSUE LOCALY.
CLINICAL FEATURES:
- PROGRESSIVE DYSPNOEA
- COUGH W3ITH SPUTUM
- CHEST SHAPE
- POOR POSTURE
- POLYCYTHEMIA
- COR PULMONALE
COMPLICATIONS:
PNEUMOTHORAX
RESPIRATORY FAILURE
CONGESTIVE CARDIAC FAILURE
PRINCIPLES OF TREATMENT:

- FLU INJECTION EVERY WINTER
- STEROIDS
- ANTIBIOTICS
- OXYGEN THERAPY
- SURGERY
PHYSIOTHERAPY:
AIMS:
- TO TEACH THE PATIENT TO BREATH WITH THE MINIMUM POSSIBLE EFFORT
- TO ESTABLISH A COORDINATED PATTERN OF BREATHING
- TO ASSIST IN THE REMOVAL OF SECRETIONS.
- TO INCREASE THE RANGE OF MOVEMENTS OF THE JOINTS
- TO INCREASE EXERCISE TOLERANCES.
- TO REGAIN FULLEST POSSIBLE FUNCTION.
ASTHMA:
ASTHMA IS THE CLINICAL SYNDROME CHARACTERISED BY ATTACKS OF WHEEZING AND BREATHLESSNESS DUE TO NARROWING OF THE PULMONARY AIRWAYS.
TYPES:
EXTRINSIC ASTHMA
INTRINSIC ASTHMA
PATHOLOGY:
- SPASM OF SMOOTH MUSCLE IN THE WALLS OF THE BRONCHI AND BRONCHIOLES.
- OEDEMA OF THE MUCUS MAMBRANE OF THE BRONCHI AND BRONCHIOLES EXCESSIVE MUCUS PRODUCTION
CLINICAL FEATURES:
EXTRINSIC ASTHMA
ONSET IS SUDDEN AND PAROXYSMAL.OFTEN AT NIGHT.AN ATTACK STARTS WITH CHEST TIGHTNESS,DRYNESS OR IRRITATION IN THE UPPER RESPIRATORY TRACT.ATTACKS MAY BE EPISODIC,OFTEN OCCURING SEVERAL TIMES A YEAR.
WHEEZE AND DYSPNOEA
COUGH IS UNPRODUCTIVE
POSTURE
PULSE IS RAPID
TACHYCARDIA
CYANOSIS
TREATMENT:GENERAL MANAGEMENT OF ASTHMATIC PATIENTS COMPRISES PREVENTION OF ATTACKS,MAINTENCE OF GENERAL FITNESS AND TREATMENT DURING AN ATTACK.
BRONCHIECTASIS :
IT IS AN ABNORMAL DIALATATION OF THE BRONCHI ASSOCIATED WITH OBSTRUCTION AND INFECTION.
TYPES:
CONGENITAL
ACQUIRED
PATHOLOGY:
BRONCHIAL OBSTRUCTION WILL CAUSE ABSORPTION OF THE AIR FROM THE LUNG TISSUE DISTAL TO THE OBSTRUCTION AND THIS AREA WILL THEREFORE SHRINK AND COLLAPSE.THIS CAUSES A TRACTION FORCETO BE EXERTED UPON THE MORE PROXIMAL AIRWAYS WHICH WILL DISTORT AND DILATE THEM.
CLINICAL FEATURES:
COUGH AND SPUTUM
DYSPNOEA
HAEMOPTYSIS
RECURRENT PNEUMONIA
HALITOSIS
CHRONIC SINUSITIS
CLUBBING
THORACIC MOBILITY
CLUBBING
COMPLICATIONS:
RECURRENT HAEMOPTYSIS
PLEURISY AND EMPYEMA
ABCESS FORMATION.
EMPHYSEMA
RESPIRATORY FAILURE
RIGHT VENTRICULAR FAILURE
RIGHT VENTRICULAR FAILURE
PNEUMONIA
PHYSIOTHERAPY:
- REMOVE SECRETIONS AND CLEAR LUNG FIELDS.
- TEACH GOOD COUGHING TECHNIQUE.
- MAINTAIN MOBILITY OF THE THORAX.
- PROMOTE GOOD GENERAL HEALTH
CYSTIC FIBROSIS
IT IS THE DISORDER OF EXOCRINE GLANDS,WITH A HIGH SODIUMCHLORIDE CONTENT IN SWEAT AND PANCREATIC INSUFFICIENCY RESULTING IN MALABSORPTION.
THERE IS HYPERTROPHY AND HYPER PLASIA OF MUCUS SECRETING GLANDS RESULTING IN EXCESSIVE MUCUS PRODUCTION IN THE LINING OF BRONCHI WHICH PREDISPOSES THE PATIENT TO CHRONIC BRONCHOPULMONARY INFECTION.
CLINICAL FEATURES:
CHILDREN:
- MECONIUM ILEUS
- FAILURE TO THRIVE AND GAIN WAIGHT.
- COUGH PRODUCING COPIOUS,OFTEN PURULENT,SPUTUM
- DYSPNOEA
- WHEEZING
- HIGH LEVEL OF SODIUM IN SWEAT
- FREQUENT,FOUL SMELLING STOOLS
ADULTS AND ADOLESCENTS:
- PROGRESSIVE BREATHLESSNESS
- REDUCED FEV1 AS CHRONIC AIRWAYS OBSTURCTION DEVELOPS.
- CONTINUED WHEEZING AND PRODUCTIVE COUGH WITH PURULENT SPUTUM
- HAEMOPTYSIS
- FINGER CLUBBING
- PUBERTY DELAYED
- INFERTILITY
COMPLICATIONS:
- HAEMOPTYSIS
- SPONTANEUS PNEUMOTHORAX
- LUNG ABCESSS,BRONCHIECTASIS
- MECONIUM ILEUS
- LIVER DISEASE.
TUBERCULOSIS
:
- Tuberculosis (TB) is a potentially fatal contagious
disease that can affect almost any part of the body but is mainly an
infection of the lungs.
- Types of TB. Tuberculosis (TB) is divided into two categories: pulmonary and extrapulmonary.
- Tuberculosis is an infection of the lungs caused by the bacterium Mycobacterium tuberculosis (M. tuberculosis).
MYOCARDIAL INFARCTION
The death of myovardial muscle cells.it occurs when myocardial ischeamia is sufficiently severe and prolong to cause irreversible damage.
Risk factors:
- FANILY HISTORY
- SERUM LIPID
- BLOOD PRESSURE
- TOBACCO CHEWING
- PHYSICAL ACTIVITY IN LEISURE
- STRESS
- OBESITY
- CLOTTING FACTORS
Management:
AIMS:
- TO KEEP THE PATIENT ALIVE
- TO RETURN HIM TO HIS NORMAL PLACE IN SOCIETY WITH AS FEW SYMPTOMS AS GOOD A PROGNOSIS AS POSSIBLE.
TREATMENT:
- REASSURANCE THAT HE CAN BE HELPED
- RELIEF OF PAIN
- DRUGS TO MAINTAIN CIRCULATION
- ADMINISTRATION OF OXIGEN
- REGULAR EXERCISES IMPROVE THE RISK OF TOLERANCE OF THE PATIENTS
- DRUGS

Arterial Thrombi

Coronary thrombosis.
When a thrombus forms within an artery, this is known as an arterial thrombosis.
Arterial thrombi:
- Usually develop on top of an atherosclerotic plaque
- Have a grey-white appearance, are firmly adherent and grow in the opposite direction from the point of attachment
- Are composed of regularly arranged layers of platelets and fibrin,
irregularly mixed with small amounts of darker red coagulated blood
containing erythrocytes
- Manifest as MI unstable angina, ischaemic stroke and some manifestations of peripheral arterial disease, such as acute limb ischaemia
-
Risk factors
Important risk factors for arterial thrombosis include:
- Smoking
- Obesity
- High blood pressure
- Increased levels of cholesterol
- Diabetes
- Increasing age
- Family history
- Physical inactivity
- Increased concentrations of blood coagulation factors
- Blood serum lipid abnormalities
Incidence and prevalence
Cardiovascular disease is the
leading cause of death in industrialized countries. Coronary artery
disease (CAD) is the most common form of cardiovascular disease. In CAD,
atherosclerosis
damages the coronary artery wall predisposing to thrombus formation.
The symptoms and severity of acute coronary syndromes (unstable angina
and MI) vary depending on the degree to which thrombi occlude the
coronary arteries.
PNEUMOTHORAX
A pneumothorax is a collection of free air in the chest
outside the lung that causes the lung to collapse.
TYPES:
A spontaneous pneumothorax, also referred to as a primary
pneumothorax, occurs in the absence of a traumatic injury to the chest or a
known lung disease. A secondary (also termed complicated) pneumothorax occurs as
a result of an underlying condition.

Physiotherapy management of patients with pneumothorax
There are no published data regarding
physiotherapy management of patients with pneumothorax. The following recommendations are based on expert opinion and clinician consensus.
Goals for Physiotherapy in Pneumothorax Treatment
- To improve distribution of ventilation
- To reinflate atelectatic lung areas
- To increase oxygenation
- Improve exercise tolerance
- Maintain airway clearance
- See more at: http://www.physiotherapy-treatment.com/pneumothorax-treatment.html#sthash.1kYpO07q.dpuf
PHYSIOTHERAPY TREATMENT:
Goals for Physiotherapy in Pneumothorax Treatment
- To improve distribution of ventilation
- To reinflate atelectatic lung areas
- To increase oxygenation
- Improve exercise tolerance
- Maintain airway clearance
- Physiotherapy Role in Small Pneumothorax Treatment
A small pneumothorax (< 3 cm apex-to-cupola distance)is not a contraindication to chest physiotherapy, but if during treatment the patient becomes more breathless or complains of chest pain the doctor should be notified immediately as it is possible that the pneumothorax could have increased in size.
If the patient has had a recent pneumothorax or a history of recurrent pneumothoraxes IPPB is probably contraindicated.
Gentle coughing can be performed and adequate humidification for ease of sputum expectoration.
Reduce exercise intensity and avoid upper limb resistance exercises.
When exercising a patient who has a small pneumothorax, or following a recent pneumothorax or haemoptysis, the physiotherapist should monitor the signs and symptoms during an exercise session.
Physiotherapy Role in Large Pneumothorax Treatment
A larger pneumothorax (> 3 cm apex-to-cupola distance) will require an intercostal drain and physiotherapy should be withheld until the drain has been inserted.
Analgesia will probably be required before treatment and the patient's usual physiotherapy regimen should be continued, but chest clapping may be unnecessary and may cause discomfort.
If the air leak persists and surgical intervention is undertaken, it is essential that physiotherapy is restarted as soon as the patient is awake postoperatively.
Adequate analgesia and humidification will assist the clearance of secretions.
Shoulder ROM exercises can be performed but avoid upper limb resistance exercises.
Aerobic exercise should be started like walking, gentle cycling etc.
Avoid positive pressure therapy while draining and for 1-2 weeks after to avoid pleural fistula and risk of recurrence.
Physiotherapy management of patients with pneumothorax
There are no published data regarding
physiotherapy management of patients with pneumothorax. The following recommendations are based on expert opinion and clinician consensus.
Goals for Physiotherapy in Pneumothorax Treatment
- To improve distribution of ventilation
- To reinflate atelectatic lung areas
- To increase oxygenation
- Improve exercise tolerance
- Maintain airway clearance
Physiotherapy Role in Small Pneumothorax Treatment
-
A small pneumothorax (< 3 cm apex-to-cupola distance)is not a
contraindication to chest physiotherapy, but if during treatment the
patient becomes more breathless or complains of chest pain the doctor should be notified immediately as it is possible that the pneumothorax could have increased in size.
- If the patient has had a recent pneumothorax or a history of recurrent pneumothoraxes IPPB is probably contraindicated.
- Gentle coughing can be performed and adequate humidification for ease of sputum expectoration.
- Reduce exercise intensity and avoid upper limb resistance exercises.
-
When exercising a patient who has a small pneumothorax, or following a
recent pneumothorax or haemoptysis, the physiotherapist should monitor
the signs and symptoms during an exercise session.
Physiotherapy Role in Large Pneumothorax Treatment
-
A larger pneumothorax (> 3 cm apex-to-cupola distance) will require
an intercostal drain and physiotherapy should be withheld until the
drain has been inserted.
- Analgesia
will probably be required before treatment and the patient's usual
physiotherapy regimen should be continued, but chest clapping may be
unnecessary and may cause discomfort.
-
If the air leak persists and surgical intervention is undertaken, it is
essential that physiotherapy is restarted as soon as the patient is
awake postoperatively.
- Adequate analgesia and humidification will assist the clearance of secretions.
- Shoulder ROM exercises can be performed but avoid upper limb resistance exercises.
- Aerobic exercise should be started like walking, gentle cycling etc.
- Avoid positive pressure therapy while draining and for 1-2 weeks after to avoid pleural fistula and risk of recurrence.
- See more at: http://www.physiotherapy-treatment.com/pneumothorax-treatment.html#sthash.1kYpO07q.dpuf
Physiotherapy management of patients with pneumothorax
There are no published data regarding
physiotherapy management of patients with pneumothorax. The following recommendations are based on expert opinion and clinician consensus.
Goals for Physiotherapy in Pneumothorax Treatment
- To improve distribution of ventilation
- To reinflate atelectatic lung areas
- To increase oxygenation
- Improve exercise tolerance
- Maintain airway clearance
Physiotherapy Role in Small Pneumothorax Treatment
-
A small pneumothorax (< 3 cm apex-to-cupola distance)is not a
contraindication to chest physiotherapy, but if during treatment the
patient becomes more breathless or complains of chest pain the doctor should be notified immediately as it is possible that the pneumothorax could have increased in size.
- If the patient has had a recent pneumothorax or a history of recurrent pneumothoraxes IPPB is probably contraindicated.
- Gentle coughing can be performed and adequate humidification for ease of sputum expectoration.
- Reduce exercise intensity and avoid upper limb resistance exercises.
-
When exercising a patient who has a small pneumothorax, or following a
recent pneumothorax or haemoptysis, the physiotherapist should monitor
the signs and symptoms during an exercise session.
Physiotherapy Role in Large Pneumothorax Treatment
-
A larger pneumothorax (> 3 cm apex-to-cupola distance) will require
an intercostal drain and physiotherapy should be withheld until the
drain has been inserted.
- Analgesia
will probably be required before treatment and the patient's usual
physiotherapy regimen should be continued, but chest clapping may be
unnecessary and may cause discomfort.
-
If the air leak persists and surgical intervention is undertaken, it is
essential that physiotherapy is restarted as soon as the patient is
awake postoperatively.
- Adequate analgesia and humidification will assist the clearance of secretions.
- Shoulder ROM exercises can be performed but avoid upper limb resistance exercises.
- Aerobic exercise should be started like walking, gentle cycling etc.
- Avoid positive pressure therapy while draining and for 1-2 weeks after to avoid pleural fistula and risk of recurrence.
- See more at: http://www.physiotherapy-treatment.com/pneumothorax-treatment.html#sthash.1kYpO07q.dpuf
Physiotherapy management of patients with pneumothorax
There are no published data regarding
physiotherapy management of patients with pneumothorax. The following recommendations are based on expert opinion and clinician consensus.
Goals for Physiotherapy in Pneumothorax Treatment
- To improve distribution of ventilation
- To reinflate atelectatic lung areas
- To increase oxygenation
- Improve exercise tolerance
- Maintain airway clearance
- See more at: http://www.physiotherapy-treatment.com/pneumothorax-treatment.html#sthash.8GYUgEt7.dpuf
PULMONARY FIBROSIS
Physiotherapy management of patients with pneumothorax
There are no published data regarding
physiotherapy management of patients with pneumothorax. The following recommendations are based on expert opinion and clinician consensus.
Goals for Physiotherapy in Pneumothorax Treatment
- To improve distribution of ventilation
- To reinflate atelectatic lung areas
- To increase oxygenation
- Improve exercise tolerance
- Maintain airway clearance
Physiotherapy Role in Small Pneumothorax Treatment
-
A small pneumothorax (< 3 cm apex-to-cupola distance)is not a
contraindication to chest physiotherapy, but if during treatment the
patient becomes more breathless or complains of chest pain the doctor should be notified immediately as it is possible that the pneumothorax could have increased in size.
- If the patient has had a recent pneumothorax or a history of recurrent pneumothoraxes IPPB is probably contraindicated.
- Gentle coughing can be performed and adequate humidification for ease of sputum expectoration.
- Reduce exercise intensity and avoid upper limb resistance exercises.
-
When exercising a patient who has a small pneumothorax, or following a
recent pneumothorax or haemoptysis, the physiotherapist should monitor
the signs and symptoms during an exercise session.
Physiotherapy Role in Large Pneumothorax Treatment
-
A larger pneumothorax (> 3 cm apex-to-cupola distance) will require
an intercostal drain and physiotherapy should be withheld until the
drain has been inserted.
- Analgesia
will probably be required before treatment and the patient's usual
physiotherapy regimen should be continued, but chest clapping may be
unnecessary and may cause discomfort.
-
If the air leak persists and surgical intervention is undertaken, it is
essential that physiotherapy is restarted as soon as the patient is
awake postoperatively.
- Adequate analgesia and humidification will assist the clearance of secretions.
- Shoulder ROM exercises can be performed but avoid upper limb resistance exercises.
- Aerobic exercise should be started like walking, gentle cycling etc.
- Avoid positive pressure therapy while draining and for 1-2 weeks after to avoid pleural fistula and risk of recurrence.
- See more at: http://www.physiotherapy-treatment.com/pneumothorax-treatment.html#sthash.1kYpO07q.dpuf
Physiotherapy management of patients with pneumothorax
There are no published data regarding
physiotherapy management of patients with pneumothorax. The following recommendations are based on expert opinion and clinician consensus.
Goals for Physiotherapy in Pneumothorax Treatment
- To improve distribution of ventilation
- To reinflate atelectatic lung areas
- To increase oxygenation
- Improve exercise tolerance
- Maintain airway clearance
Physiotherapy Role in Small Pneumothorax Treatment
-
A small pneumothorax (< 3 cm apex-to-cupola distance)is not a
contraindication to chest physiotherapy, but if during treatment the
patient becomes more breathless or complains of chest pain the doctor should be notified immediately as it is possible that the pneumothorax could have increased in size.
- If the patient has had a recent pneumothorax or a history of recurrent pneumothoraxes IPPB is probably contraindicated.
- Gentle coughing can be performed and adequate humidification for ease of sputum expectoration.
- Reduce exercise intensity and avoid upper limb resistance exercises.
-
When exercising a patient who has a small pneumothorax, or following a
recent pneumothorax or haemoptysis, the physiotherapist should monitor
the signs and symptoms during an exercise session.
Physiotherapy Role in Large Pneumothorax Treatment
-
A larger pneumothorax (> 3 cm apex-to-cupola distance) will require
an intercostal drain and physiotherapy should be withheld until the
drain has been inserted.
- Analgesia
will probably be required before treatment and the patient's usual
physiotherapy regimen should be continued, but chest clapping may be
unnecessary and may cause discomfort.
-
If the air leak persists and surgical intervention is undertaken, it is
essential that physiotherapy is restarted as soon as the patient is
awake postoperatively.
- Adequate analgesia and humidification will assist the clearance of secretions.
- Shoulder ROM exercises can be performed but avoid upper limb resistance exercises.
- Aerobic exercise should be started like walking, gentle cycling etc.
- Avoid positive pressure therapy while draining and for 1-2 weeks after to avoid pleural fistula and risk of recurrence.
Book Appointment
Consult Dr Prodyut Das (PT)
HOD Physiotherapy & Fitness center
NIMT Hospital, Greater Noida
Former Physio ISIC Hospital
(+919910883909)
Blog & News
Branches
Links
Author's Pick
SITE MAP
You liked it? then do share
Testimonials
"Physiotherapy Treatment Approach continues
to exceed my expectations in terms of the quality that Prodyut continues
to put out there. This is the leading website in the world in regards
to progressing our understanding of human movement and how we apply it
to the rehabilitation and strength and conditioning setting. Keep up the
good work Prodyut!"
- Dave O'Sullivan, Physical Therapist
"Continue your great work-love your site! It
has sent me in new directions as a PT -love looking at different points
of view and see how I can incorporate it into my practice!"
- Kenny Physical Therapist, UK
"Prodyut Das has put together a fantastic
resource for any professional involved in the rehabilitation or
performance training of athletes. physiotherapy-treatment.com has
become my go-to resource for cutting edge information on elite athletic
development and injury prevention."
- Emmannual Augustine, Physiotherapist, ISIC, New Delhi, India.
Average Rating- 4.5
Votes- 187
- See more at: http://www.physiotherapy-treatment.com/pneumothorax-treatment.html#sthash.1kYpO07q.dpuf
Pulmonary fibrosis is the formation or development of excess fibrous connective tissue (fibrosis) in the lungs. It is also described as "scarring of the lung"
.
There are many potential causes of pulmonary fibrosis, such as:
- rheumatoid arthritis
- scleroderma
- lupus
- mineral dusts - coal, silicon, asbestos (asbestosis), metals
- poisonous industrial gases such as chlorine and sulphur dioxide
- radiation treatment to the chest
- poisons - particularly paraquat
- medications (e.g., nitrofurantoin, amiodarone, bleomycin, cyclophosphamide methotrexate)
Symptoms and Complications of Pulmonary Fibrosis
For the
majority of people, the symptoms of pulmonary fibrosis come on slowly
over the course of months to years, but for some people the symptoms can
develop more rapidly.
Most people with pulmonary fibrosis
first see their doctor about increasing shortness of breath during
exercise. Some also have a cough. These are often the only symptoms of
early pulmonary fibrosis, but you might also feel one or more of the
following symptoms:
- loss of stamina
- loss of appetite
- fatigue
- weight loss
- diffuse chest pain
Later on, symptoms can include:
- shortness of breath without exercise - eating, talking, or just resting
- cyanosis (blue lips, nail beds, and sometimes skin due to lack of oxygen in the tissue)
- clubbing of the fingers (enlarged fingertips)

ARDS (Acute Respiratory Distress Syndrome)
Acute respiratory distress syndrome (ARDS)
is a rapidly developing, life-threatening condition in which the lung
is injured to the point where it can't properly do its job of moving air
in and out of the blood.
Conditions that can directly injure the lungs and possibly lead to ARDS include:
- Breathing in smoke or poisonous chemicals
- Breathing in stomach contents while throwing up (aspiration)
- Near drowning
-
Pneumonia
- Severe acute respiratory syndrome (SARS), a lung infection
Conditions that can indirectly injure the lungs and possibly lead to ARDS include:

- Bacterial blood infection (sepsis)
- Drug overdose
- Having many blood transfusions
- Heart-lung bypass
- Infection or irritation of the pancreas (pancreatitis)
- Severe bleeding from a traumatic injury (such as a car accident)
- Severe hit to the chest or head
ARDS is defined by three main signs and symptoms:
- Rapid breathing
- Feeling like you can't get enough air in your lungs
- Low oxygen levels in your blood, which can lead to organ
failure and symptoms such as rapid heart rate, abnormal heart rhythms,
confusion, and extreme tiredness
- The aims of physiotherapy are:
-
Passive/Active movements
-
Chest Physiotherapy in this case involve four principal manoeuvers:
-
Positioning to enhance the removal of secretions and to improve gas exchange
-
Manual Hyperinfl
-
Removal of retained secreations
- ation
-
Endotracheal suction
-
Manual techniques which include shakings and vibrations
-
Passive and active exercises need to be performed regularly whilst the
patient mobility remain restricted during the critical stages of their
disease, in order to maintain the mobility of joints and extensibility
of soft tissues (e.g. muscles, tendons and ligaments).
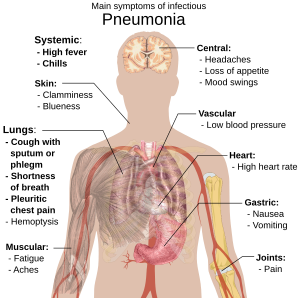
PMEUMONIA
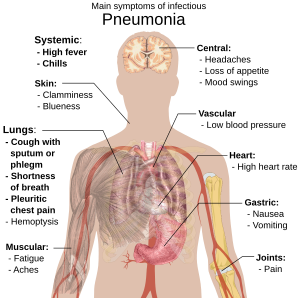
PHYSIOTHERAPY TREATMENT:
-HUMIDIFICATION-steam inhalation and nebulization to moistem & clear ling fields secreations.
-Clapping,shaking,& breathing exercise
-Postural drainage in different positions
-Chest expersion exercise
-Exercise tolerance & fitness training.
HUMIDIFICATION-steam inhalation and nebulization to moistem & clear ling fields secreations.
-Clapping,shaking,& breathing exercise
-Postural drainage in different positions
-Chest expersion exercise
-Exercise tolerance & fitness training.