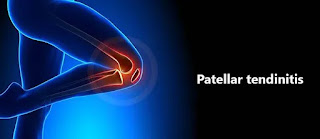
What is patellar tendinitis?
Patellar 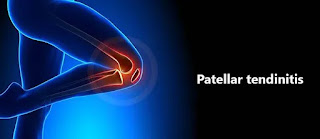 |
| Patellar tendinitis |
tendinitis is an injury to the tendon connecting your kneecap (patella) to your shinbone (tibia). The patellar tendon works with the muscles at the front of your thigh to straighten your knee so that you can kick, run and jump.
Patellar tendinitis is also termed a jumper’s knee. This condition is most common in athletes whose sports involve frequent jumping — sports like basketball and volleyball. However, it is not such that a person who is in sports activity suffer from a condition,, even people who don’t participate in jumping sports can get patellar tendinitis.
Patellar tendonitis condition happens when the patellar tendon becomes inflamed (swollen) or irritated. It is due to overuse or repetitive activity. It typically affects athletes
For most people, treatment of patellar tendinitis starts with physical therapy to stretch and strengthen the muscles around the knee joint.
Patellar tendonitis is also called a:
- Patellar tendinosis
- Patellar tendinopathy
- Jumper’s knee
Patellar tendonitis develops slowly. The condition becomes more severe each time the tendon is overstressed or overused, so it is essential for a person to rest their knee after each injury. Rest will give the body time to heal.
What is a Patellar tendon?
The quadriceps is a muscle whose tendon is located just above the kneecap (patella). The quadriceps tendon connects the quadriceps muscles to the top of the kneecap on the anterior side of the thigh. The patellar tendon is situated just below the kneecap, which connects the kneecap (patella) to the shinbone (tibia). The function of the quadriceps tendon and patellar tendon is to work with the muscles in the front of the thigh to extend or straighten the knee. Therefore, both tendons are important in permitting people to perform activities such as climbing stairs, walking, running, and jumping.
Despite its name, the patellar tendon is truly a ligament. Anatomically, tendons connect a muscle to a bone and ligaments connect two muscles.
The patellar tendon provides stability to the knee joint, holding bones together. It also works in a team with the quadriceps (thigh) muscle and other connective tissues to help in moving. A person couldn’t straighten their knee or jump without it.
What are the Causes of Patellar Tendinitis?
Patellar tendonitis happens when there is more stress on knee tendon tissues, or someone walks too fast, over and over again. Repeated jumping and springing motions stress and strain the bands of patellar tendon tissues. Over time, lots of minor strains and tiny tears make the tendon tissues weaker and sore.
This injury happens slowly over a long time. There may be two main types of activities that damage tendon tissues:
Sudden, increase in activity (how much you’re jumping).
Returning to play at full strength after a long break instead of slowly getting back into your regular routine.
Patellar tendonitis occurs due to repetitive stress on the knee, most often due to overuse in sports or exercise. The repetitive stress on the knee creates tiny tears in the tendon that, over time, inflame and later on weaken the tendon.
Contributing factors can be:
- Tight leg muscles
- Uneven leg muscle strength
- Misaligned feet, ankles, and legs such as Knee Valgus Deformity
- Obesity
- Shoes without enough padding
- Hard playing surfaces
- Chronic diseases that weaken the tendon
Athletes are more at risk because running, jumping, and squatting put more stress on the patellar tendon. For example, running, or walking can put a force of up to five times more than your body weight on your knees.
If patellar tendonitis remains untreated, a person may have a risk of tendon tear. A large tear of the patella tendon is a serious injury, and a complete tear will separate the patellar tendon from the kneecap. They may hear a tearing or popping sound and feel significant pain when moving.
In a jumper’s knee, it is caused by overuse of your knee joint, such as regular jumping on hard surfaces.
It’s usually a sports-related injury, related to leg muscle contraction and the force of hitting the ground. This force strains the tendon. With repeated stress, a tendon may become inflamed.
Symptoms:
The following are the symptoms:
- Pain: Pain is the main symptom of patellar tendinitis, usually present between your kneecap and the point where the tendon attaches to your shinbone (tibia).
- Pain may be a dull type just below the kneecap
- Pain while jumping, running, or walking
- Pain when bending or straightening your leg from sitting or standing
- Kneeling down or getting up from a squatting position can be especially painful.
- Swelling: The painful tendon may appear thickened or swollen compared to the non-affected tendon on another side.
- Tenderness around the knee
- Stiffness: The tendon can often feel unbendable initially in the morning or after physical activity.
Initially, a person may only feel pain in the knee as they begin physical activity or just after an intense workout. Over a long time, the pain progressively worsens and starts to interfere while playing sports like basketball, and volleyball. Later on, the pain interferes with daily and routine movements such as climbing stairs or rising from a chair.
Diagnosis:
It is important not to ignore ongoing pain or discomfort in the knee. Identifying patellar tendonitis early means the condition will be easier and faster to treat, reducing a person’s risk of serious injury.
During the examination, the doctor may apply pressure to parts of your knee to determine where you feel pain. Usually, pain occurs from patellar tendinitis on the front part of your knee, just below your kneecap.
A doctor will ask about:
- Physical activity
- what symptoms patient experiencing
- When the symptoms occur
- What remedy you’ve tried that eases the pain
The doctor will test the range of motion of the knee by bending and extending the leg.
A doctor may also perform other imaging tests to look at your kneecap and tendon to determine if there is any damage to the tendon or bone. These tests can also help to rule out other possible causes of your pain, such as a fracture or any other condition.
Your doctor may perform:
X-ray: A X-ray to look at the bone to determine whether they have a kneecap fracture or if your kneecap is displaced.
MRI: A MRI to look at the tendon and show any damage to the soft tissue in the knee joint
Ultrasound: An ultrasound to look at the tendon and show any soft tissue damage. Reveal any tears in joint
Complications:
If they do have not medical treatment, patellar tendonitis can worsen. They may damage their tendon more severely, limiting everyday functioning.
Resting legs and stopping activity can be emotionally challenging for athletes, in particular. They may not desire to stop playing, even though it is painful. For professional athletes, patellar tendonitis can be a career-ender if it is left untreated.
Treatment:
Home treatment:
Home remedies
If you have pain in the knee, consider the following:
Pain relievers. Over-the-counter medications such as ibuprofen and naproxen sodium and NSAIDs may provide short-term pain relief.
Avoid activity that causes pain. A person may need to practice their sport less often or temporarily switch to a lower-impact sport. Working or walking with pain can further damage a patellar tendon.
Ice. Apply ice after activity for 10 minutes if that causes pain. Place ice in a plastic bag and wrap the bag in a towel and keep it on the pain area. Or try an ice massage on it. It will reduce swelling and pain.
Medical treatment:
If home remedies do not work, then the person should consult with a doctor for complete treatment. The doctor may provide a pain reliever. It may provide short-term relief from the pain associated with patellar tendinitis.
The doctor may prescribe over-the-counter (OTC) drugs for short-term pain and inflammation reduction.
These can include drugs such as:
- Ibuprofen
- Naproxen sodium
- Acetaminophen
If knee pain is severe, your doctor may give you a corticosteroid injection in the area around the patellar tendon. This treatment is more effective in reducing severe pain. It may also weaken the tendon and possibly make it more likely to rupture. So, it’s important to put considerable thought into this treatment and its associated risks.
Another way of delivering corticosteroid drugs is by spreading the drug over the knee and using a low electrical charge to push it through the skin. This way is called iontophoresis.
Surgical and other procedures
If conservative treatments do not work, the doctor may suggest other therapies, such as:
Corticosteroid injection: An ultrasound-guided corticosteroid injection is injected into the sheath around the patellar tendon may help in relieving pain. But these types of drugs also have complications such as can also weaken tendons and making them more likely to rupture.
Platelet- Rich Plasma injection: This type of injection has been tested in some people with chronic patellar tendon problems. It is hoped the injections might promote new tissue formation and help in healing damage in the tendon.
Oscillating needle procedure. This procedure is performed using local anesthesia. The doctor uses ultrasound imaging to guide a small oscillating needle that cuts away the damaged area while sparing a healthy tendon. This is a fairly new procedure.
Surgery: Surgery is needed in rare cases, if other treatments fail and are successful in relieving pain, the doctor might suggest surgical debridement of the patellar tendon. These procedures can be done through small incisions around the knee.
Traditional surgery involves opening the knee to scrape the damaged knee cap and tendon. More recently, arthroscopic surgery is used for this process. This involves making only four small incisions in the knee, and it has a shorter recovery time, so heals faster.
Recovery time after surgery varies. Some surgical protocols instruct immobility in a cast after your operation. Another strategy for healing suggests that a forceful and immediate rehabilitation exercise program works excellently. In this protocol, people were able to return to high-level activity in 3 months to a year.
Physical Therapy:
The aim of physical therapy is to decrease pain and inflammation. If your pain is unbearable even while you are resting your legs. The doctor may recommend that to support your leg by wearing a brace and using crutches for a while to avoid further damage to the tendon. When movements are relatively pain-free, you can begin physical therapy activities.
Physical therapy can help restore movement gradually as the tendon heals. A physical therapist may also recommend strengthening and stretching exercises people can do at home to do activities without pain in the future.
Additionally, a physical therapist can help in controlling re-injury by finding the cause of the tendonitis. To do this, the doctor can examine a person’s movement patterns and determine why the tendons are being overloaded or overstressed again and again. For example, if a person has weakness in the hips, the knees may take more of the impact when running or jumping, which can cause pain.
In rare cases, untreated tendonitis can lead to a complete tear in the tendon. If this happens, a person may need surgical treatment to reattach the tendon to the bone.
A physical therapy session generally includes:
- A warm-up period
- Ice or massage for your knee
- Stretching exercises
- Strengthening exercises
Modalities: Modalities such as ultrasound and electrical stimulation are used to ease your knee pain.
Supportive device: A knee brace or taping of your knee may help in reducing pain when you are exercising by keeping the kneecap in place.
A physical therapist will develop an exercise program for you that may include the following exercises:
Stretching
Isometric exercises, where your joint angle and muscle length remain fixed but contractions happen. This exercise helps in relieving pain.
Eccentric exercises are squats performed on a decline board
Flexibility exercises for the thigh and calf muscle
An alternative method of treatments
Exercises and stretches
Doing the exercise in the wrong way, or doing too much too soon, can cause additional damage. People should exercise carefully and do gentle exercises and progress slowly.
Some examples of exercises that may be helpful are given below:
Seated hamstring stretch
Hamstring stretch can be done by sitting on the floor, and stretching one leg straight in front. Keeping the leg straight and toes pointed upwards, gently bend towards the foot. Hold this stretch position for 30 seconds at a time. Can do it 5 times and repeat on both legs.
Quad stretch |
| Quad stretch |
In a side-lying position, keep the affected knee flexed and extend as possible by using your hand. Hold this position for 30 seconds and 5 times. Slowly remove the force from the leg and repeat on the other side.
Wall Squats |
| Wall Squats |
Stand with the feet shoulder-width apart while your Back is supported with a wall. Keeping the back straight and neck up, slowly bend from the knees while engaging the glutes. Go as low as you are comfortable. Repeat exercise 8–10 times.
Alternatively or by modifying, a person can try a decline squat by keeping their heels on a small block or thick book. This takes some of the strain off the patellar tendons when performing squatting exercises.
Supine leg lifts
In the supine position, lie on the back with the legs extended up and straight. Slowly lower one leg while keeping the knee in the extended position, then activate the quads to lift the leg. Repeat this exercise on each side.
How to Prevent Patellar Tendinitis?
After an individual has recovered from patellar tendonitis condition, they can take a few steps to prevent future injuries.
The following are prevention for athletes to reduce their risk of injury:
- Warming up and stretching before starting the exercise
- Cooling down and stretching after doing exercise
- Wearing knee support such as a brace when playing sports
- Knee Exercises to strengthen the leg muscles and support the knees
- Avoiding jumping, running, and landing on very hard surfaces, such as concrete
Recovery time:
Recovery time for patellar tendonitis varies. It depends on how severely a person has an injury, their overall health and age, and how they treat the condition.
If a person has mild tendonitis, they may be able to return to their normal activities in 3-4 weeks, and in more severe cases, it may take 3 months or more to gets heal.
Some people have pain in their knees even after recovering from patellar tendonitis. Although pain is usually mild and effortless, persistent tendonitis can prevent a person from doing certain activities.
For some athletes, the condition may be chronic. For others, the therapy enables a return to normal functioning and sports.
Important factors in recovery are:
- Attaching to your rehabilitation program and regularly exercising
- Resuming your sports activity gradually
- Paying attention to pain, and resting as required
- Using Over Counter remedies and ice to help with returning pain
Summary:
Patellar tendonitis is a common knee injury among athletes involving repetitive running and jumping. This stress on the knee damages the patellar tendon, causing pain and inflammation.
The outlook for patellar tendonitis varies based on the severity of the injury. It is such a common occurrence for runners and other athletes.
Patellar tendonitis can develop slowly, so it can be difficult to recognize at first. A person with continued discomfort or pain in the knee should contact a doctor to evaluate their pain.
Resting and supporting by bracing the knee gives a tendon time to heal. In mild cases, patellar tendonitis heals in a few weeks but if the pain continues, a doctor or physical therapist can recommend further treatment options
The best treatment for this condition is to take rest and avoid activities that might aggravate the condition. Doctors may also recommend physical therapy exercises, modifying activities, home treatment-ice and heat, and painkillers.