|
| Low Back pain |
Low back pain is a general term for pain in your lower back (the part of your spine between your pelvis and your tailbone). It can be acute or chronic. Acute low back pain usually lasts for less than three months, while chronic low back pain lasts for more than three months.
Low back pain is a common condition that affects a large number of people worldwide. For many people, lower back pain can make everyday activities difficult. It's important to understand the causes of this low back pain and find ways to relieve them.
There are several factors that contribute to low back pain, but most cases have an underlying problem. The most common issues include: Lifestyle and the way you take care of yourself, Body Mechanics: Poor muscle strength in your low back, Muscle Imbalance - in which one muscle is stronger than another, Joint abnormalities (such as arthritis), Disc injuries or conditions that can cause pain in the discs between your vertebrae.
Sufferers of low back pain may feel pain in the lower part of their back, though it may radiate down their leg and into the knee. The cause of low back pain is typically a combination of factors such as poor posture that has been incorrectly strengthened through repetitive movements, prolonged sitting at one position, overuse of the spine muscles, abnormal mechanics in the spine or another joint area such as when a person presses their knees together while standing.
The lower back is made up of 5 lumbar vertebrae — L1 through L5 — which are joined together by discs and ligaments. These vertebrae provide stability and support to the spine. The discs act like shock absorbers, cushioning the spine and helping it move naturally when put under stress.
The main function of your lower back is to support your upper body by holding up your spine. When you bend over to pick up something heavy or lean over to reach something on a higher shelf, your legs must use their muscles to help lift you up and your arms must be used to push yourself forward. Your legs are also used for running or other activities that require quick movements. When you sit at a desk all day long or stand for long periods of time, it's important that you have strong muscles in your legs and core so that you can support yourself against gravity.
Low back pain can happen when any part of the spine bends too far forward from its normal position — this can include putting too much weight on one leg while standing or leaning forward from a sitting position
In this post, we cover the causes of low back pain, common symptoms, diagnosis and treatment. We explain what can determine whether you have lumbar spondylytic or herniated disk, and give some suggestions on how to reduce pain in the short term. We also talk about exercise, ergonomics, and diet. The post concludes with a short section on exercises to improve core strength when suffering with low back pain.
- Section: What is low back pain?
- Section: Causes of low back pain
- Section: Symptoms of low back pain
- Section: Diagnosis of low back pain
- Section: Treatment of low back pain
- Section: Exercise for low back pain
- Section: Ergonomic tips for prevention of low back pain
Takeaway: Taking care of your lower back is important for your health and quality of life.
What Is Low Back Pain?
Low back pain is a common condition that affects a large number of people in worldwide. For many people, lower back pain can make everyday activities difficult. It's important to understand the causes of this low back pain and find ways to relieve them.
Low back pain is usually caused by inflammation or irritation in the muscles, joints, ligaments, tendons, or nerves that support the spine. When these structures become irritated or inflamed, they cause pain and stiffness in the area where they are located. This is also known as referred pain.
What Causes Low Back Pain?
The main cause of low back pain can be due to an injury or illness, or it may be related to other conditions such as arthritis, degenerative disc disease, or chronic fatigue syndrome. In some cases, low back pain may be caused by long-term stress or anxiety. These factors can all affect the way your body responds to injury, illness, or other stressful events.
The most common causes are:
- Degenerative changes in the bones and joints of the spine
- Muscle weakness or spasms that limit movement
- Injuries to muscles and ligaments around the spine, such as broken bones or torn ligaments
- Injury or strain to lower back muscles
- Poor posture
- Lack of exercise and/or physical activity
- Age-related wear and tear of the spine
- Stress
other causes are:
Herniated discs: These lumps or bulges in the center of your vertebrae are caused by pressure from the surrounding tissues pushing on them from all sides. Herniated discs are very painful and may also cause sciatica (pain down one or both legs).
Spinal stenosis: This condition occurs when there's too much pressure on one side of your spinal column, which can lead to nerve compression and nerves being pinched off by bone spurs or other structures in the spine
Poor posture: Many people with low back pain have trouble with their posture. This is because they tend to slouch when they're sitting or standing up, which puts extra stress on the muscles and joints in their lower backs. Some people also experience pain when they get up from a sitting position, especially if they have weak abdominal muscles may lead to lumbar lordosis posture (the muscles around your abdomen).
Stress fractures: Fractures that occur as a result of trauma, such as falls or car accidents, are also known as stress fractures.
Stress injuries: These can occur after strenuous activity, such as running up stairs or lifting weights at the gym
Symptoms include:
- Pain in one or both buttocks and/or thighs
- Pain radiating down into one or both legs
- Pain that gets worse with activity
- Pain that wakes you up at night
- Tenderness to touch over the spine
- A feeling of stiffness or tightness in the lower back
- Difficulty maintaining balance while standing or walking
- Constipation
Diagnosis:
If you have been experiencing lower back pain for more than 3 weeks, you should see your doctor for an evaluation. An evaluation may include imaging tests such as X-rays or MRIs (magnetic resonance imaging). These images will help doctors determine if there is any damage to your spine and whether or not you have any conditions that would require further treatment.
Your doctor will perform a physical exam.
X-rays show the bones of the spine, discs, and joints that can cause pain if there is damage to these structures. They are usually taken when you stand upright.
MRIs (magnetic resonance imaging) have a stronger pull on the spine than X-rays do, so they can better detect damage to your spine’s soft tissues.
CT (computed tomography) scan
Ultrasonography and Bone density tests also help to diagnose the Low back pain
Low Back Pain Treatment Options
In some cases, treating low back pain with physical therapy can help improve the strength and flexibility of your muscles and ligaments. Other treatments include:
Medication - Pain medications such as acetaminophen (Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs) may relieve muscle aches and joint stiffness associated with low back pain. If over-the-counter medications don't provide adequate relief after several weeks, talk with your doctor about using prescription drugs such as ibuprofen
A nerve block can be used to help relieve pain from compression on the nerves in your spine. This may include injections with steroids and anesthetic medications into specific areas along the spine where there is pressure from compressed nerves (epidural space).
Your doctor may recommend that you wear a brace or splint to provide support while your back heals itself over time.
If you have back pain that doesn’t respond to non-surgical treatments, surgery may be recommended.
 |
| Low Back pain exercise |
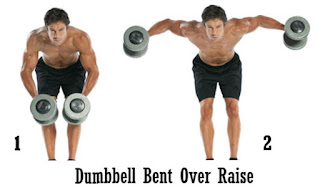
The physiotherapy treatment for low back pain includes exercise, physical therapy, and other treatments to relieve discomfort in your back and spine. Exercise may include stretching exercises or strengthening exercises for the muscles around your pelvis and hips that support your spine.
Physical therapy focuses on the movement and function of your spine and muscles. A physical therapist can help with exercises that strengthen the core muscles around your pelvis and back to prevent pain.
Physiotherapy is a back pain treatment that helps reduce pain and restore function. It can help in improving the quality of life by reducing the disability and making sure that you get back to your regular day-to-day activities.
There are a number of exercises that are recommended by physiotherapists to make sure that you recover from back pain. These exercises include strengthening, stretching, aerobic, and core exercises. You can also use heat therapy, hydrotherapy, massage therapy, and acupuncture to reduce the pain.
You will be guided on how to do the exercises and give advice on which methods are more effective. You should not attempt these exercises without consulting a physiotherapist. Massage therapy, acupuncture, heat therapy, hydrotherapy, and exercise programs are also recommended.